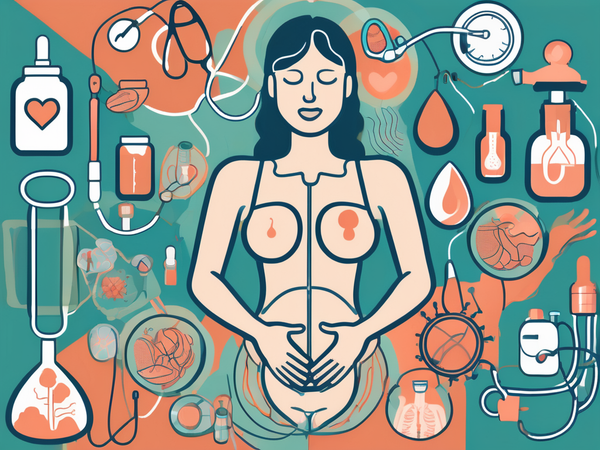
PCOS or Polycystic Ovary Syndrome, is a common endocrine disorder that affects many women around the world. It is characterized by hormonal imbalances, which can lead to various symptoms and potential complications. Understanding PCOS is crucial for early detection, diagnosis, and effective management of this condition.
Understanding PCOS
Defining PCOS: A Brief Overview
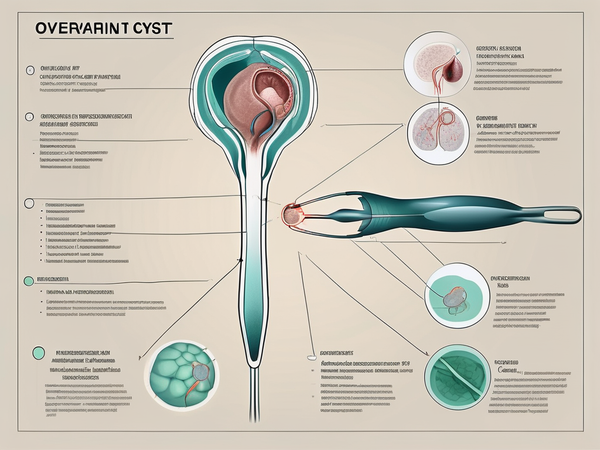
PCOS is a complex disorder that affects the female reproductive system. It is characterized by enlarged ovaries containing small cysts or follicles. These cysts are often the result of hormonal imbalances, particularly elevated levels of androgens or male hormones, such as testosterone.
While the exact cause of PCOS is unknown, genetic and environmental factors are believed to play a role. Additionally, insulin resistance has been observed in many women with PCOS, which can further disrupt hormone levels and worsen symptoms.
PCOS can manifest in a variety of symptoms, including irregular menstrual cycles, infertility, weight gain, acne, and excessive hair growth (hirsutism). The condition can also increase the risk of developing other health issues, such as type 2 diabetes, high blood pressure, and cardiovascular disease.
The Science Behind PCOS: Causes and Risk Factors
Researchers have identified several potential causes and risk factors for PCOS. These include;
- Genetics or family history
- Insulin resistance
- Obesity
- Hormonal imbalances
Insulin resistance, commonly associated with obesity, can also contribute to the development of PCOS by affecting the body's ability to regulate hormones.
Hormonal imbalances, specifically elevated levels of androgens and insulin, play a significant role in the development of PCOS. Androgens are male hormones that are also present in females but in smaller amounts. When these levels are elevated, they can disrupt the normal function of the ovaries and lead to the characteristic symptoms of PCOS. Insulin, a hormone that helps regulate blood sugar levels, can also impact hormone production when the body becomes resistant to its effects.
Recognizing PCOS
Common Signs and Symptoms
PCOS presents with a wide range of signs and symptoms, which can vary in severity between individuals. Common symptoms include:
- Irregular or absent menstrual periods
- Excessive hair growth (hirsutism)
- Facial Acne
- Excessive Hair Fall
- Weight gain or difficulty losing weight
- Fertility problems
- Mood Swings
Additionally, many women with PCOS may experience mood swings, depression, and anxiety.
It's important to note that PCOS is a complex hormonal disorder that affects about 1 in 10 women of childbearing age. The exact cause of PCOS is not fully understood, but it is believed to involve a combination of genetic and environmental factors. Women with PCOS often have higher-than-normal levels of androgens, which are sometimes referred to as male hormones, although all women produce androgens to some extent.
At What Age Does PCOS Typically Start?
PCOS can develop at any age after the start of menstruation. However, it is most commonly diagnosed during a woman's late teens or early twenties. Early detection is crucial, as it allows for timely intervention and management to minimize the impact on reproductive and overall health.
It's worth mentioning that PCOS is a leading cause of female infertility due to the hormonal imbalances and irregular ovulation associated with the condition. Women with PCOS may have difficulty conceiving and may require medical assistance to achieve pregnancy. It's recommended that women with PCOS work closely with healthcare providers specializing in reproductive health to explore treatment options tailored to their individual needs.
Diagnosing PCOS
Medical Tests and Procedures
Diagnosing PCOS involves a comprehensive approach that combines medical history assessment, physical examination, and various diagnostic tests. When you visit your healthcare provider for concerns related to PCOS, they will likely start by gathering information about your symptoms, menstrual history, and any family history of PCOS. This initial assessment helps in understanding your unique situation and provides valuable insights for further evaluation.
During the physical examination, your healthcare provider will carefully check for physical signs that are commonly associated with PCOS, such as excessive hair growth, acne, and enlarged ovaries. These indicators, along with the information obtained from your medical history, play a crucial role in the diagnostic process.
Additionally, to confirm the presence of PCOS, your healthcare provider may recommend further tests. These can include blood tests to assess hormone levels, ultrasound imaging to visualize the ovaries, and in some cases, additional tests to exclude other conditions that may mimic PCOS symptoms. By conducting these tests, healthcare providers can gather more data to make an accurate diagnosis and tailor a suitable treatment plan.
Interpreting Results and Confirming Diagnosis
Interpreting the results of the diagnostic tests is a key step in confirming a diagnosis of PCOS. Your healthcare provider will carefully analyze the hormone levels and ultrasound findings to identify specific patterns that are indicative of PCOS. Typically, a diagnosis is considered when at least two of the following criteria are met: irregular or absent menstrual periods, elevated androgen levels, and the presence of polycystic ovaries on ultrasound.
Treating PCOS
Medical Treatments and Procedures
PCOS treatment aims to manage the symptoms and minimize associated health risks. Depending on the individual's goals and specific symptoms, medical treatments may include hormonal contraceptives to regulate menstrual cycles, anti-androgen medications to reduce excessive hair growth, and insulin-sensitizing medications to improve insulin resistance.
In some cases, fertility treatments may be necessary for women trying to conceive. These can include ovulation induction medications or in vitro fertilization (IVF) procedures. It is essential to consult with a healthcare professional to determine the most appropriate treatment plan based on individual needs and goals.
Furthermore, surgical options such as ovarian drilling may be considered in cases where medication and lifestyle changes have not been effective in managing PCOS symptoms. Ovarian drilling is a minimally invasive procedure that involves using heat or laser to destroy a portion of the ovary, which can help restore ovulation in some women with PCOS.
Living with PCOS
Management Strategies for PCOS
Living with Polycystic Ovary Syndrome (PCOS) requires ongoing self-care and management strategies. This can involve monitoring and tracking menstrual cycles, maintaining a healthy lifestyle, and attending regular check-ups with healthcare providers.
Lifestyle Changes and Natural Remedies
Alongside medical treatments, lifestyle changes can have a significant impact on the management of PCOS.
Weight Balance: Maintaining a healthy weight through a balanced diet. A modest weight loss can also improve your symptoms to a greater extent.
Regular Exercise: Regular exercise can help improve insulin sensitivity and hormone balance. Individuals with PCOS must pay close attention to their diet and exercise routines, as weight management plays a significant role in managing symptoms such as irregular periods, acne, and excessive hair growth.
No Stress: Additionally, managing stress levels, getting enough sleep, and incorporating relaxation techniques can further support overall well-being.
Clean Habits: Avoid drinking and smoking as the carcinogens present in them further deteriorate the cystic conditions of the ovaries.
Moreover, certain natural remedies and supplements have shown promise in managing PCOS symptoms. For example, Myo-inositol, a type of B vitamin, has been found to help improve insulin sensitivity and regulate menstrual cycles in women with PCOS. Similarly, acupuncture and herbal remedies such as chasteberry and saw palmetto may offer benefits in addressing hormonal imbalances associated with PCOS.
In addition to physical health, mental well-being is also a crucial aspect of managing PCOS. Incorporating stress-reducing activities such as yoga, meditation, or counseling can help individuals better cope with the emotional challenges that often accompany this condition. Support from friends, family, or online communities can provide a sense of belonging and understanding, making the journey with PCOS feel less isolating.
Long-Term Health Considerations
While PCOS is a manageable condition, it is essential to be aware of potential long-term health considerations. Women with PCOS have a higher risk of developing type 2 diabetes, cardiovascular disease, and endometrial cancer. This increased risk underscores the importance of adopting a proactive approach to health management. Regular health screenings, such as blood sugar monitoring, lipid profiles, and gynecologic exams, are crucial for early detection and prevention of these potential complications.
Furthermore, hormonal imbalances associated with PCOS can impact fertility and reproductive health. Individuals with PCOS who are planning to conceive may face challenges such as irregular ovulation. In such cases, working closely with a healthcare provider or fertility specialist can help explore options such as ovulation induction or assisted reproductive technologies to improve the chances of successful conception.
Supplements for PCOS
Various supplements comprising a combination of hormonal balance herbs such as Shatavari, Inositols, Chasteberry, Licorice, and many other herbs are available for managing PCOS symptoms. It is ideal to go for a highly bioavailable combination of these powerful herbs along with inositols for best results.
Conclusion
PCOS is a complex disorder that affects many women worldwide. Understanding the causes, symptoms, and available treatment options is crucial for the proper management of this condition. By working closely with healthcare providers, making lifestyle changes, and staying proactive in self-care, women with PCOS can lead healthy and fulfilling lives.