Understanding PCOS and Breastfeeding
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that affects many women during their reproductive years. While PCOS is primarily known for its impact on fertility, it can also have implications for breastfeeding. Understanding how PCOS affects breastfeeding is crucial for new mothers with this condition.
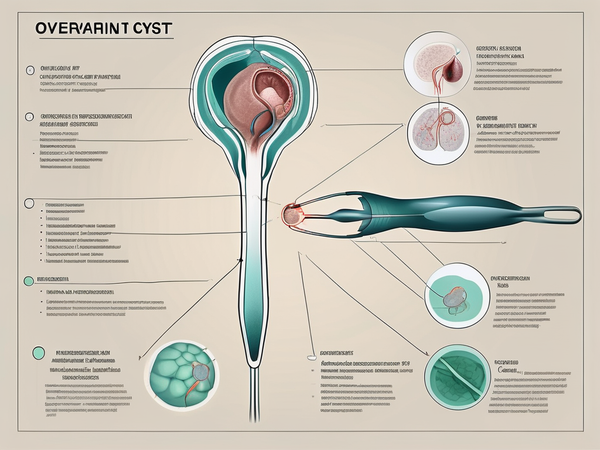
PCOS is characterized by an imbalance in reproductive hormones, which can lead to irregular menstrual cycles, ovarian cysts, and insulin resistance. These hormonal changes can affect the production and quality of breast milk, making breastfeeding challenging for some women with PCOS.
The Impact of PCOS on Breastfeeding
One of the primary ways PCOS can affect breastfeeding is by reducing milk supply. Women with PCOS may experience difficulties in establishing and maintaining an adequate milk supply, which can lead to frustration and stress for both mother and baby.
The hormonal imbalances associated with PCOS can interfere with the release of prolactin, the hormone responsible for milk production. This can result in a decreased supply of breast milk and difficulty in sustaining exclusive breastfeeding.
In addition to reduced milk supply, women with PCOS may also face challenges such as delayed onset of lactation and slower weight gain in their infants. These factors can further complicate the breastfeeding journey.
The Connection Between PCOS and Breast Milk Supply
Research suggests that the impaired insulin signaling associated with PCOS may play a role in the reduced milk supply experienced by some women. Insulin resistance can affect the production and transport of lactose, the primary carbohydrate in breast milk. This disruption in lactose metabolism can lead to decreased milk production.
Furthermore, women with PCOS are more likely to have elevated levels of androgens, such as testosterone. These hormones can interfere with prolactin production and inhibit milk synthesis. The combination of hormonal imbalances and insulin resistance can thus contribute to the challenges faced by women with PCOS when it comes to breastfeeding.
Women with PCOS need to work closely with healthcare professionals, such as lactation consultants and endocrinologists, to navigate the complexities of breastfeeding. These experts can guide techniques to increase milk supply, such as frequent breastfeeding or pumping, as well as offer support and reassurance throughout the breastfeeding journey.
Additionally, implementing lifestyle changes, such as maintaining a healthy diet, exercising regularly, and managing stress levels, can also have a positive impact on breastfeeding for women with PCOS. These lifestyle modifications can help regulate hormone levels and improve overall well-being, potentially enhancing milk production and breastfeeding success.
Breast Changes During Pregnancy
Pregnancy is a time of significant changes for a woman's body, including the breasts. Understanding these changes is essential for new mothers, as they directly impact breastfeeding.
Hormonal Changes and Their Effects
During pregnancy, hormones such as estrogen and progesterone surge, preparing the breasts for lactation. These hormones stimulate the growth and development of mammary gland tissue, leading to an increase in breast size. The increased blood flow to the breasts also causes them to feel swollen and tender.
But what exactly do these hormones do?
Estrogen is responsible for the growth of milk ducts, while progesterone helps in the formation of lobules, the structures that produce milk. Together, they create the perfect environment for breastfeeding.
These hormonal changes are crucial for the initiation of lactation but may also cause discomfort and sensitivity in the breasts. Expectant mothers need to be aware of these changes and seek appropriate support and guidance to manage any discomfort.
Physical Changes in the Breasts
Alongside hormonal changes, physical changes occur in the breasts to prepare for breastfeeding. The milk ducts enlarge and branch out, forming a complex network that will transport the milk from the glands to the nipple.
But that's not all! As the breasts prepare for their new role, they also change their appearance. The areolas, the darker area around the nipples, may become larger and more pronounced. This is nature's way of ensuring that newborns can easily locate the source of nourishment.
Colostrum, a thick and yellowish fluid rich in antibodies and nutrients, is generated in the breasts during late pregnancy. This serves as the first milk for the newborn and provides essential immune protection in the early days of life.
As the due date approaches, the breasts may start to produce and leak colostrum. This is a normal physiological response and indicates that the breasts are preparing to provide nourishment for the baby.
So the changes in the breasts during pregnancy are not only hormonal but also physical. They are a testament to the incredible journey of motherhood and the body's remarkable ability to adapt and nurture new life.
Blood Sugar Regulation and Breastfeeding
Understanding the role of blood sugar in lactation can provide valuable insights. Blood sugar levels play a crucial role in optimal lactation. Fluctuations in blood sugar can impact milk production and hinder breastfeeding success. Women with PCOS, who often have difficulties regulating blood sugar, may face additional challenges in maintaining an adequate milk supply.
Supplements for Enhancing Breastfeeding
In addition to understanding the effects of PCOS and the changes that occur during pregnancy, several supplements can support breastfeeding. These supplements address various aspects of lactation, including milk supply, blood sugar regulation, and milk production.
Metformin: In addition to blood sugar regulation, another supplement that has shown potential benefits for breastfeeding is metformin. It is clinically shown to improve breastfeeding. Metformin is a medication commonly prescribed to manage insulin resistance in women with PCOS. However, it is crucial to consult with a healthcare provider before starting or continuing metformin while breastfeeding. The dosage and timing of metformin administration may need to be adjusted to ensure the safety of both mother and baby.
Magnesium: Another key supplement for lactation is magnesium. Supplementing with magnesium may help improve milk supply in women with PCOS. Adequate magnesium levels are necessary for the synthesis and release of prolactin, the hormone responsible for milk production. However, it is important to work with a healthcare provider to determine the appropriate dosage and form of magnesium supplement for individual needs.
Galactagogues: Galactagogues are substances that are believed to enhance milk production. Some commonly used galactagogues include herbs like fenugreek, blessed thistle, and fennel. These herbs have been traditionally used to stimulate milk supply and promote lactation.
While galactagogues can be helpful for some women, it is important to note that their effectiveness varies from person to person. Consulting with a lactation specialist or healthcare provider can help determine the suitability and dosage of galactagogues for your specific needs.
Techniques for Improving Breastfeeding
In addition to supplements, various techniques can aid in improving breastfeeding for women with PCOS. These techniques focus on enhancing milk flow and establishing a strong bond between mother and baby.
The Importance of Skin-to-Skin Contact
Skin-to-skin contact, also known as kangaroo care, is a technique that involves placing the newborn on the mother's bare chest immediately after birth. This practice has numerous benefits, including promoting breastfeeding initiation, regulating temperature, and fostering bonding.
For women with PCOS, skin-to-skin contact can help stimulate the release of hormones like oxytocin, which is crucial for milk let-down. It also provides an opportunity for the baby to latch on and establish effective breastfeeding.
Breast Massage: A Natural Way to Enhance Milk Flow
Breast massage is another technique that can be beneficial for improving milk flow and relieving any discomfort associated with engorgement or blocked ducts. Gentle massaging of the breasts before and during breastfeeding can help stimulate milk flow and ensure efficient milk transfer.
Massaging the breasts also helps increase blood flow to the mammary glands, delivering more nutrients and oxygen to support milk production. It is essential to use proper techniques and seek guidance from a lactation specialist to avoid any potential harm or discomfort.
Conclusion