PCOS is a complex hormonal condition that has major consequences on women's overall health, physical as well as emotional. Many lifestyle disorders like diabetes, hypertension, and thyroid can occur, if PCOS is not handled properly.
Understanding PCOS and its Long-Term Impact
PCOS (Polycystic Ovarian Syndrome) is a prevalent hormonal disorder affecting women of reproductive ages, with an estimated 5-10% worldwide prevalence. It is characterized by hormonal imbalance and ovarian dysfunction, leading to various health concerns such as impaired glucose tolerance. diabetes, and cardiovascular complications. The exact cause of PCOS remains unclear, necessitating further research for effective diagnosis and management strategies. Genetic and environmental factors also contribute to the development, making diagnosis and management challenging.
It is important to note that PCOS not only affects women of reproductive age but can also have implications for adolescents and postmenopausal women. Early detection and intervention are crucial in managing the symptoms and preventing potential long-term health consequences associated with PCOS.
The Long-Term Health Implications of PCOS
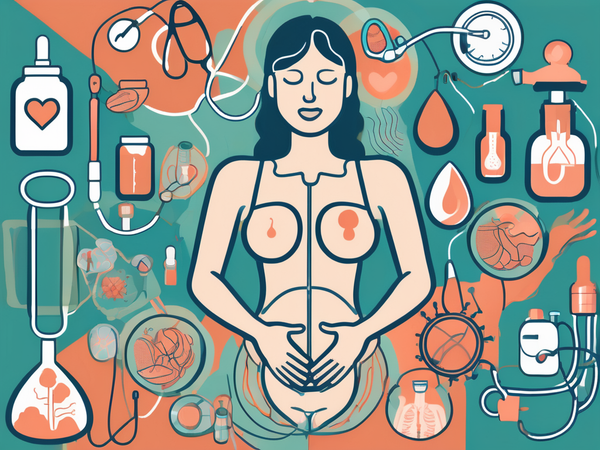
PCOS can have profound effects on a woman's long-term health. Women with PCOS have an increased risk of developing various health conditions, including impaired glucose tolerance and diabetes, sleep apnea, hypertension, cardiovascular complications, thyroid disorders, and certain types of cancer.
Regular monitoring and comprehensive care are essential for women with PCOS to mitigate the risks of these long-term health implications. A multidisciplinary approach involving gynecologists, endocrinologists, nutritionists, and mental health professionals is often recommended to address the diverse needs of individuals with PCOS and improve their overall quality of life.
PCOS Impaired Glucose Tolerance & Diabetes
Impaired glucose tolerance and diabetes are common comorbidities of PCOS, contributing to the long-term health risks associated with the condition.
The Connection Between PCOS and Glucose Tolerance
Women with PCOS often exhibit insulin resistance, which impairs the body's ability to properly utilize glucose. This insulin resistance can lead to elevated blood sugar levels and an increased risk of impaired glucose tolerance and diabetes.
How PCOS Increases the Risk of Diabetes
The hormonal imbalances and insulin resistance seen in PCOS can contribute to the development of type 2 diabetes. Furthermore, research has shown that the presence of PCOS can exacerbate the progression of impaired glucose tolerance to diabetes. The chronic inflammation associated with PCOS can further worsen insulin resistance, making it crucial for individuals with PCOS to prioritize managing their blood sugar levels. Women with PCOS should closely monitor their blood sugar levels and adopt a healthy lifestyle that includes regular physical activity and a balanced diet to reduce their risk of developing diabetes.
Healthcare providers need to screen individuals with PCOS for glucose intolerance regularly. Early detection and intervention can help prevent or delay the onset of diabetes in these individuals. By addressing the underlying insulin resistance through targeted lifestyle modifications and, in some cases, medication, the risk of developing diabetes can be significantly reduced.
PCOS and Sleep Apnea
Research suggests that there is a strong association between PCOS and sleep apnea. Hormonal imbalances, obesity, and insulin resistance commonly seen in PCOS can contribute to the development of sleep disorders.
Sleep apnea, a sleep disorder characterized by interruptions in breathing during sleep, is another health issue that can arise in women with PCOS.
Women with PCOS already face a myriad of challenges due to hormonal imbalances, particularly elevated levels of androgens (male hormones) and insulin resistance can disrupt the normal sleep cycle and increase the risk of developing sleep apnea. Furthermore, the excess weight often carried by women with PCOS can exacerbate the symptoms of sleep apnea. Excess fat around the neck and throat area can put pressure on the airway, leading to breathing difficulties during sleep. This highlights the importance of weight management in the treatment and prevention of sleep apnea in women with PCOS.
Understanding the Impact of Sleep Apnea in Women with PCOS
Sleep apnea can have detrimental effects on overall health, including reduced quality of sleep, daytime fatigue, and an increased risk of cardiovascular complications. Women with PCOS should be aware of the potential link between the condition and sleep apnea and seek appropriate diagnosis and treatment if symptoms arise.
Healthcare providers must screen women with PCOS for sleep apnea to ensure early detection and intervention. By addressing both PCOS and sleep apnea simultaneously, healthcare professionals can improve the quality of life and overall health outcomes for women dealing with these interconnected conditions.
Hypertension: A Common Issue in PCOS Patients
Hypertension, or high blood pressure, is prevalent among women with PCOS and requires careful management.
Polycystic Ovary Syndrome (PCOS) is a common endocrine disorder affecting women of reproductive age, also associated with various metabolic abnormalities, including hypertension.
Studies have shown that women with PCOS have a higher prevalence of hypertension compared to those without the condition. The exact mechanisms behind this association are not yet fully understood, but hormonal imbalances, insulin resistance, and obesity are believed to play a role.
Furthermore, the chronic low-grade inflammation commonly seen in PCOS may contribute to the development of hypertension. This inflammatory state, characterized by elevated levels of certain cytokines and other inflammatory markers, can lead to endothelial dysfunction and arterial stiffness, both of which are risk factors for high blood pressure.
Managing Hypertension in Women with PCOS
Management of hypertension in women with PCOS involves lifestyle modifications, such as regular exercise, a healthy diet, and weight management. In some cases, medication may be necessary to control blood pressure levels effectively. Regular monitoring and maintenance of healthy blood pressure are essential for preventing long-term cardiovascular complications.
In addition to traditional approaches to managing hypertension, women with PCOS may benefit from specific interventions targeting the underlying hormonal and metabolic disturbances associated with the condition. For example, medications that help regulate insulin levels, such as metformin, have been shown to improve blood pressure control in women with PCOS and hypertension.
Cardiovascular Complications Associated with PCOS
Women with PCOS have an increased risk of developing cardiovascular complications, highlighting the need for proactive management and preventive measures.
Why PCOS Increases Cardiovascular Risk
The hormonal imbalances and metabolic disturbances seen in PCOS, including insulin resistance and dyslipidemia, contribute to an increased risk of cardiovascular complications. These complications can include heart disease, stroke, and even heart attacks.
Preventing Cardiovascular Complications in PCOS Patients
Preventing cardiovascular complications in women with PCOS involves adopting a heart-healthy lifestyle, which includes regular exercise, a balanced diet, weight management, stress reduction, and quitting smoking. Regular cardiovascular screenings and early intervention are crucial to reducing the long-term impacts of PCOS on heart health.
Thyroid, Ovarian Cancer, and Breast Cancer
PCOS has also been associated with an increased risk of thyroid disorders, ovarian cancer, and breast cancer.
Thyroid Disorders in PCOS
Research suggests that there is a higher prevalence of thyroid disorders, such as hypothyroidism, in women with PCOS. Regular thyroid function monitoring and appropriate management are essential to maintain overall health.
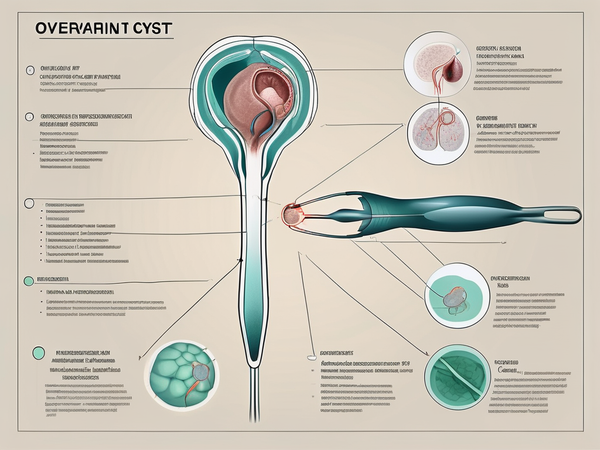
Ovarian Cancer and PCOS
While more research is needed to establish a conclusive link, some studies have suggested an association between PCOS and an increased risk of ovarian cancer. Women with PCOS should discuss their individual risk factors and appropriate screening options with their healthcare providers.
Breast Cancer and PCOS
Although the relationship between PCOS and breast cancer is still under investigation, hormonal imbalances and insulin resistance seen in PCOS may influence breast cancer risk. Regular breast self-examinations and mammograms as recommended by healthcare professionals are crucial for early detection and treatment.
Conclusion
Polycystic Ovary Syndrome (PCOS) has far-reaching effects on women's health and requires a multidisciplinary approach to long-term management. A comprehensive understanding of the potential implications of PCOS can aid in early detection, timely intervention, and the adoption of preventive measures. By addressing the various components of PCOS, including impaired glucose tolerance, sleep apnea, hypertension, cardiovascular complications, thyroid disorders, and potential cancer risks, women with PCOS can take actionable steps toward improving their overall health and minimizing the long-term impact of this complex hormonal disorder.