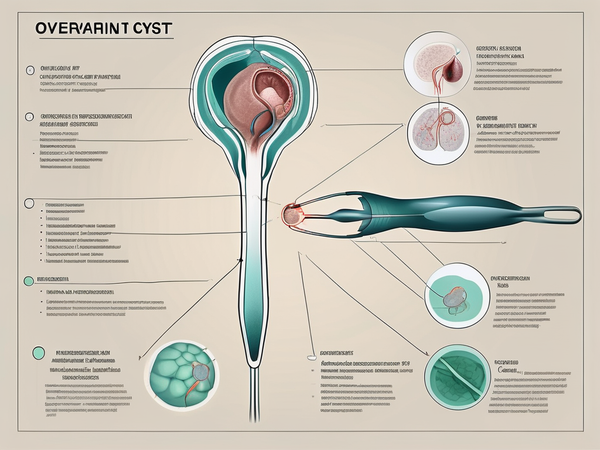
Polycystic ovary syndrome (PCOS) is a common hormonal disorder that affects women of reproductive age. It is characterized by the presence of cysts on the ovaries, irregular menstrual cycles, and excessive production of androgens, the male hormones. PCOS can have a significant impact on fertility, making it difficult for women to conceive naturally. However. it is not a prominent cause, women can still get pregnant up to a great extent.
PCOS affects approximately 5-10% of women and is one of the leading causes of infertility. Understanding how PCOS occurs and its effect on ovulation is crucial in managing this condition and improving fertility outcomes.
Defining PCOS: A Brief Overview
PCOS is a complex hormonal disorder with a range of symptoms that can vary from woman to woman. The exact cause of PCOS is unknown, but it is believed to be influenced by a combination of genetic and environmental factors.
Diagnosing PCOS involves assessing a woman's symptoms, conducting a physical examination, and performing blood tests to measure hormone levels. The presence of cysts on the ovaries can be identified through an ultrasound scan.
The Biological Mechanism of PCOS
PCOS is characterized by an imbalance in hormone levels, particularly elevated levels of insulin and androgens. Insulin resistance, a condition where the body's cells do not respond properly to insulin, is a common feature of PCOS.
Insulin resistance leads to increased insulin production, which in turn stimulates the ovaries to produce excessive amounts of androgens. This hormonal imbalance disrupts the normal ovulation process, leading to irregular menstrual cycles and difficulty in conceiving.
PCOS and Its Effect on the Ovulation Process
PCOS and ovulation are directly linked together. Ovulation is the process by which a mature egg is released from the ovary. In women with PCOS, the hormonal imbalance interferes with ovulation, causing irregular or absent menstrual cycles. This irregularity makes it difficult to predict when ovulation will occur, making it challenging for women with PCOS to conceive naturally.
Furthermore, the presence of cysts on the ovaries can further hinder the release of mature eggs. Without regular ovulation, the chances of fertilization and pregnancy are significantly reduced.
It is important to note that PCOS not only affects fertility but also has other potential health implications. Women with PCOS are at a higher risk of developing conditions such as type 2 diabetes, high blood pressure, and heart disease. Therefore, managing PCOS goes beyond improving fertility outcomes; it involves addressing the overall health and well-being of women with this condition.
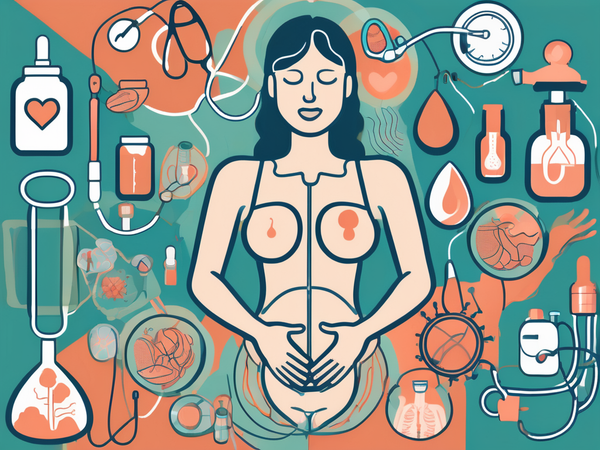
The Relationship Between PCOS and Pregnancy
PCOS can present unique challenges during pregnancy. Women with PCOS have a higher risk of developing gestational diabetes, high blood pressure, and preeclampsia during pregnancy. These conditions can have adverse effects on both the mother and the developing baby. Hence, in some women, PCOS and pregnancy go parallelly.
Additionally, women with PCOS have an increased likelihood of miscarriage and premature birth. The hormonal imbalances associated with PCOS can affect the development of the pregnancy, increasing the risk of complications.
The Challenges of PCOS During Pregnancy
Pregnancy can exacerbate the symptoms of PCOS, including insulin resistance and hormonal imbalances. Managing blood sugar levels becomes crucial to prevent complications such as gestational diabetes. Close monitoring by healthcare providers is essential throughout the pregnancy to ensure the well-being of both the mother and the baby.
Women with PCOS may also face challenges in maintaining a healthy weight during pregnancy. Weight management is important, as excessive weight gain can further complicate the pregnancy and increase the risk of gestational diabetes and other complications.
The Role of PCOS in Pregnancy Complications
PCOS is associated with an increased risk of various pregnancy complications.
Gestational Diabetes: Women with PCOS have a higher likelihood of developing gestational diabetes, a condition characterized by high blood sugar levels during pregnancy. Gestational diabetes can affect the health of the baby and increase the risk of delivery complications.
High Blood Pressure: Additionally, women with PCOS are more prone to developing high blood pressure and preeclampsia during pregnancy. These conditions can lead to complications for both the mother and the baby, including the risk of premature birth.
Fertility Issues: Furthermore, PCOS can impact the overall fertility of women, making it more challenging to conceive. The hormonal imbalances and irregular menstrual cycles associated with PCOS can make it difficult for women to predict ovulation and increase the time it takes to achieve a successful pregnancy.
Deformities: The hormonal imbalances in PCOS can affect the development of the baby's organs and systems. Studies have shown that babies born to mothers with PCOS may have a higher risk of metabolic disorders, such as obesity and insulin resistance, later in life.
Women with PCOS need to work closely with their healthcare providers to manage their condition and optimize their chances of a healthy pregnancy. Regular prenatal care, including monitoring blood sugar levels, blood pressure, and overall health, can help mitigate the risks associated with PCOS during pregnancy.
PCOS and Endometriosis
Endometriosis is a chronic condition in which tissue similar to the lining of the uterus, called endometrium, grows outside the uterus, commonly on the ovaries, fallopian tubes, and other pelvic organs. This abnormal growth can cause inflammation, pain, and the formation of scar tissue, leading to complications such as infertility. Endometriosis is often associated with PCOS. While the exact link between endometriosis and PCOS is not fully understood, both conditions can affect hormonal balance and menstrual cycles, potentially impacting fertility. Additionally, women with PCOS may have a higher risk of developing endometriosis, further complicating fertility issues. Treatment options for both conditions may include hormone therapy, surgery, and assisted reproductive techniques to manage symptoms and improve fertility outcomes.
PCOS and Gestational Diabetes
Women with PCOS have an increased risk of developing gestational diabetes during pregnancy due to underlying insulin resistance and hormonal imbalance. In PCOS, insulin resistance is very common, where the body's cells become less responsive to insulin, leading to elevated blood sugar levels. During pregnancy, hormonal changes further increase insulin resistance, increasing the likelihood of developing gestational diabetes. Thus, PCOS and diabetes are also an important link to understand and consider.
Exploring Fertility Treatment Options for PCOS
While PCOS can make it challenging to conceive naturally, there are various fertility treatment options available that can help women with PCOS achieve pregnancy.
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that affects reproductive-age women. It is characterized by irregular menstrual cycles, high levels of androgens (male hormones), and multiple small cysts on the ovaries. These hormonal imbalances can disrupt ovulation and make it difficult for women with PCOS to get pregnant.
The Role of Medication in PCOS Fertility Treatment
Medication is often used as a first-line treatment for women with PCOS who are trying to conceive. The primary goal of medication is to regulate hormone levels, induce ovulation, and improve the chances of pregnancy.
Commonly prescribed medications for PCOS include clomiphene citrate, letrozole, and metformin. These medications work by stimulating the ovaries to release mature eggs and promoting regular ovulation.
Women with PCOS need to work closely with a healthcare provider to monitor their response to medication and adjust the treatment plan as needed. Regular monitoring through blood tests and ultrasounds can help determine the optimal timing for ovulation and increase the chances of successful conception.
Surgical Treatments for PCOS-Related Infertility
In cases where medication fails to induce ovulation or the presence of certain structural abnormalities, surgical interventions may be considered.
Ovarian Drilling: A procedure performed using a laparoscope, involves making tiny holes in the ovaries to reduce androgen production and stimulate ovulation. This procedure is effective in restoring fertility outcomes in women with PCOS.
In Vitro Fertilization: IVF can be an option for women with PCOS-related infertility who have failed to conceive through other treatments. It involves fertilizing eggs with sperm outside the body and implanting the resulting embryos into the uterus, bypassing ovulation issues associated with PCOS.
Surgical treatments for PCOS-related infertility are usually considered when other treatment options have been unsuccessful. Women need to discuss the risks and benefits of surgical interventions with their healthcare provider to make an informed decision about their fertility treatment plan.
Effective Management Strategies for Infertility Due to PCOS
Managing PCOS infertility symptoms involves a multifaceted approach, combining lifestyle modifications and medical interventions. By addressing the underlying hormonal imbalances and improving overall health, women with PCOS can increase their chances of conceiving.
Lifestyle Modifications for Managing PCOS
Adopting a healthy lifestyle can significantly impact fertility outcomes for women with PCOS.
Regular Exercise: Regular aerobic exercises like cycling or swimming, combined with strength training can help manage PCOS symptoms.
A Balanced Diet: A diet rich in whole grains, and micronutrients like vitamins and minerals is essential for improving overall health. There are various forms of diet for PCOS one can refer to.
Weight Management: Losing even a small amount of weight can help regulate hormone levels and restore regular ovulation.
Furthermore, managing stress levels and getting enough sleep are also crucial in maintaining hormonal balance and overall well-being.
Medical Interventions for PCOS-Induced Infertility
In addition to lifestyle modifications, medical interventions can be used to address specific fertility concerns related to PCOS. In-vitro fertilization (IVF) may be recommended for women with PCOS who have not responded to other treatments or have additional fertility factors.
IVF involves the retrieval of eggs from the ovaries, fertilizing them with sperm in a laboratory, and transferring the resulting embryos back into the uterus. This technique can bypass the difficulties associated with PCOS-induced infertility and increase the chances of pregnancy.
Conclusion
PCOS and infertility can be challenging, but with the right management strategies and treatment options, women with PCOS can increase their chances of conception. Ongoing research and advancements in medical technology continue to improve fertility outcomes for women with PCOS.






















 DOWNLOAD NOW
DOWNLOAD NOW
