In recent years, the prevalence of PCOS and obesity has been steadily increasing, posing a significant challenge to women's health. PCOS is a hormonal disorder that affects the reproductive system, while obesity refers to the condition of having excess body fat. While these two conditions may seem unrelated at first, further examination reveals a complex interplay between them.
Understanding PCOS and Obesity
Before we delve into the connection between PCOS and obesity, it is essential to understand these conditions individually.
Polycystic Ovary Syndrome (PCOS) is a multifaceted hormonal disorder that impacts women of reproductive age worldwide. Beyond its hallmark symptoms of irregular menstrual cycles, excessive hair growth, acne, and cystic ovaries, PCOS can also manifest in insidious ways, affecting fertility and metabolic health. Studies have shown that women with PCOS have a higher prevalence of insulin resistance, which can lead to complications such as type 2 diabetes and cardiovascular issues.
Defining PCOS and Its Symptoms
PCOS, a prevalent hormonal condition in women of reproductive age, brings irregular menstrual cycles, excess hair growth, and cystic ovaries due to hormonal imbalances. Weight management struggles are frequent among those with PCOS, prompting inquiry into the relationship between the condition and obesity. Additionally, the visible symptoms and fertility concerns associated with PCOS can profoundly affect a woman's self-esteem and mental health.
The Meaning and Implications of Obesity
Obesity, on the other hand, refers to the condition of having a body mass index (BMI) above the normal range. It is associated with an increased risk of various health problems, including cardiovascular disease, diabetes, and certain types of cancer.
Obesity can arise from multiple factors, such as genetic predisposition, sedentary lifestyle, and dietary habits. While it is a complex condition influenced by various factors, research has indicated a significant association between obesity and PCOS.
Furthermore, obesity is not solely a physical health issue; it can also impact mental health and quality of life. The societal stigma and discrimination faced by individuals with obesity can lead to feelings of shame, low self-esteem, and even depression. Addressing obesity requires a holistic approach that considers both the physical and emotional well-being of individuals affected by this condition.
The Connection Between PCOS and Obesity
The Role of Insulin Resistance in PCOS and Obesity
Insulin resistance, a condition in which the body's cells become less responsive to insulin, plays a crucial role in both PCOS and obesity. Insulin resistance is often present in women with PCOS and can contribute to weight gain and difficulty losing weight.
Insulin is a hormone that regulates blood sugar levels. When cells become resistant to its effects, the body compensates by producing higher levels of insulin, which promotes fat storage and can lead to weight gain.
Furthermore, insulin resistance can also disrupt the balance of other hormones in the body, such as androgens, which are typically elevated in women with PCOS. This hormonal imbalance can further exacerbate symptoms and contribute to weight gain.
The Impact of Weight on PCOS Symptoms
Weight gain, particularly excess abdominal fat, can exacerbate the symptoms of PCOS. Increased fat stores release more hormones and chemicals that disrupt hormonal balance, leading to a vicious cycle of weight gain and worsening PCOS symptoms.
Moreover, excess weight not only affects physical health but can also have a significant impact on emotional well-being. Women with PCOS who struggle with obesity may experience low self-esteem, depression, and anxiety due to the challenges of managing their weight and dealing with the symptoms of the condition.
Additionally, excess weight can further contribute to insulin resistance, perpetuating the difficulties associated with weight management in women with PCOS. This complex interplay between weight, insulin resistance, and hormonal imbalance underscores the importance of a holistic approach to managing PCOS that includes lifestyle modifications, such as a balanced diet and regular exercise, to improve both physical and emotional health.
The Causal Relationship Between Obesity and PCOS
Exploring the Obesity-PCOS Connection
While obesity and PCOS often coexist, the exact causal relationship between them is still a topic of ongoing research. Some studies suggest that obesity may precede the development of PCOS, as increased fat tissue can affect hormone production and metabolic processes, leading to PCOS symptoms.
However, it is important to note that not all women with PCOS are obese, nor are all obese women affected by PCOS, indicating that other contributing factors are involved.
Further research is being conducted to understand the intricate interplay between obesity and PCOS. Studies are exploring how excess adipose tissue, particularly visceral fat, can influence insulin resistance and inflammation, which are key factors in the development and progression of PCOS.
Risk Factors Associated with PCOS-Related Weight Gain
Women suffering from PCOS are more likely to develop obesity along with the following risk factors including:
- Type 2 Diabetes
- Sleep Apnea
- Infertility
- High Cholesterol
- High Blood Pressure
- Endometrial cancer
PCOS and Its Potential to Cause Obesity
The Role of PCOS in Weight Gain
While obesity is recognized as a risk factor for PCOS, it is also important to consider the role of PCOS itself in weight gain. Hormonal imbalances associated with PCOS can affect metabolism, appetite regulation, and fat distribution, all of which can contribute to weight gain.
Additionally, the emotional and psychological impact of living with PCOS can lead to stress, emotional eating, and further challenges in weight management.
Women with PCOS often experience higher levels of androgens, such as testosterone, which can lead to increased abdominal fat deposition. This type of fat distribution, known as central or visceral obesity, is particularly concerning as it is associated with a higher risk of metabolic complications, such as insulin resistance and cardiovascular disease.
Hormonal Imbalance, Appetite, and PCOS
Understanding Hormonal Imbalance in PCOS
Hormonal imbalances play a central role in the development and progression of PCOS. Elevated levels of androgens, such as testosterone, can disrupt the delicate hormonal balance in the body.
This can lead to an increased appetite, particularly for foods high in carbohydrates and unhealthy fats, further contributing to weight gain.
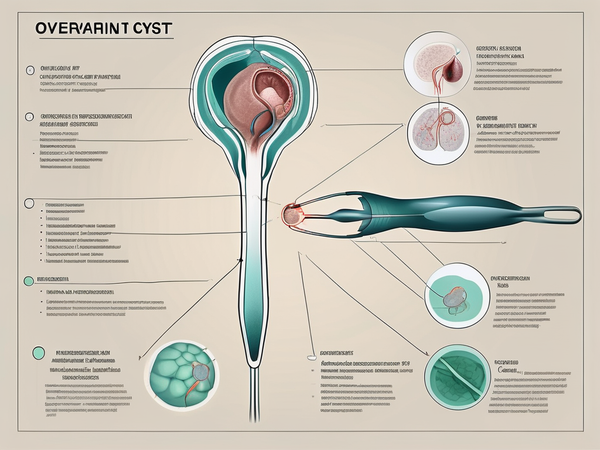
PCOS, or Polycystic Ovary Syndrome, is a common endocrine disorder that affects women of reproductive age. It is characterized by hormonal imbalances, irregular menstrual cycles, and the development of small fluid-filled sacs in the ovaries.
The Effect of Hormonal Imbalance on Appetite
Hormonal imbalances associated with PCOS can influence appetite regulation. For some women with PCOS, the hormonal disruptions can lead to an increased feeling of hunger, making it more challenging to maintain a healthy diet and promote weight loss.
Furthermore, hormonal imbalances can affect the fullness and satisfaction signals sent to the brain, leading to overeating and a lack of satiety.
Insulin resistance, commonly seen in women with PCOS, can also play a role in increased appetite. When cells become resistant to insulin, the body produces more insulin to compensate, which can stimulate appetite and lead to overeating.
How to Manage PCOS Obesity
While PCOS-related obesity presents unique challenges, there are effective strategies to manage and improve overall health.
- Adopting a balanced and nutritious diet based on whole foods, including plenty of fruits, vegetables, lean proteins, and whole grains, can help stabilize blood sugar levels, manage weight, and improve PCOS symptoms.
- Incorporating regular physical activity into daily routines can support weight management, improve insulin sensitivity, and enhance overall well-being. Activities such as aerobic exercises, strength training, and yoga have shown positive effects in women with PCOS.
- Working with healthcare professionals who specialize in PCOS can provide personalized guidance and support. They can help address hormonal imbalances, develop targeted treatment plans, and offer emotional support.
Conclusion
In conclusion, the connection between PCOS and obesity is a complex relationship influenced by hormonal imbalances, insulin resistance, and a range of other factors. While it is clear that PCOS and obesity often coexist, one does not always cause the other. Understanding and addressing the interplay between PCOS and obesity is crucial for effective management and improved overall health.